
Table of Contents
What is depression? A question that is being asked more as the illness becomes more and more prevalent. With depression seeming to become more common, it’s important for us to acknowledge how serious an issue depression is. We care so much when our bodies are going through a physical ailment, but what about our minds?
Depression is a complex, yet common mental illness which can affect all genders, ages, and backgrounds. Also known as major depressive disorder or clinical depression, depression is a mood disorder which leaves individuals with a recurring feeling of sadness and/or loss of interest in things they once enjoyed. Not to be confused with general grief, depression can have a severe impact on the way an individual feels, thinks and handles regular activities for prolonged periods of time. Unfortunately, depression is not just something you can snap out of and requires an individual to understand what they’re dealing with so that they can seek out the necessary help or medical treatment[1]. Coming to terms with what you’re feeling is hard but understand that you are not alone in this and there are so many ways to help you overcome this period of your life.
What Types of Depression Are There?[2]
Disruptive Mood Dysregulation Disorder
DMDD is a relatively new diagnosis and is a childhood condition that consists of extreme anger, irritability and frequent temper outbursts. Even though temper outbursts can be considered normal for children, DMDD is severe to the point that it hinders the child’s ability to function at school, home and with their friends.
The criteria to diagnose DMDD include:
- Severe recurring verbal rage outbursts and/or physical aggression towards people and/or property that are disproportionate to the intensity of the situation that they are reacting to.
- The temper outbursts are inconsistent with the child’s developmental level.
- The temper outbursts occur three or more times per week, on average.
- Between temper outbursts, the mood is persistently irritated and angry most of the day, nearly every day. The mood is noticeable to others such as teachers, parents and peers.
- Symptoms 1-4 have been existing for 12 or more months. Throughout that period, the individual has not lasted longer than three months consecutively without the symptoms 1-4.
- Symptoms 1 and 4 occur in at least two of three settings such as at school, at home and amongst peers and the symptoms are severe in at least one of these two.
- DMDD should not be diagnosed before the age of 6 or after the age of 18.
- The onset of symptoms 1-5 occur before the age of 10.
- There has not been a distinct period lasting more than one day in which the full symptom criteria (except duration) has been met for a manic or hypomanic episode.
- The extreme behaviors cannot be explained by other mental disorders and do not occur solely during an episode of major depressive disorder.
- The symptoms are not due to side effects of a substance or neurological condition.
How common is DMDD?
DMDD is not to be confused with other related conditions such as pediatric bipolar disorder. DMDD is common among children who visit pediatric mental health clinics. It is estimated that 2-5% children and adolescents have 6 months to 1 year period prevalence of DMDD. However, the rates are anticipated to be higher in males and school aged children than adolescents and females.
Risk Factors
- Genetics and physiology – Having a family background in which anxiety disorders, unipolar depressive disorders or substance abuse has occurred.
- Being Temperamental – Children with DMDD typically have a psychiatric history in which chronic irritability has been present before all symptoms have manifested.
- DMDD is more likely to occur in males.
Comorbidity
Rates of comorbidity is very high in relation to DMDD. It is not common to find individuals whose symptoms only relate to DMDD. Many children will present to the clinic with a wide range of disruptive behavior varying from anxiety, mood and even autism spectrum symptoms, causing overlaps with other pediatric mental disorders such as oppositional defiant disorder. Nevertheless, if a child diagnosed with DMDD is displaying symptoms that meet the criteria for bipolar disorder, then they should be diagnosed with bipolar disorder instead. Furthermore, DMDD should not be diagnosed if the symptoms only manifest when the child is put in an anxiety inducing situation.

Major Depressive Disorder
What are the symptoms of Major Depressive Disorder?
- Depressed mood most of the day, nearly every day
- Irritability
- Emptiness
- Hopelessness
- Loss of interest or pleasure
- Change in appetite or weight
- Sleeping too much or too little
- Appearing more restless or slowed down
- Feeling tired/ no energy
- Feelings of worthlessness or guilt
- Struggle to concentrate or make decisions
- Thoughts of death/suicide and attempts
Diagnosis and course of Major Depressive Disorder
In order to be diagnosed with Major Depressive Disorder, at least 5 or more of the symptoms listed above must be present during the same two-week period and one of these symptoms must be either depressed mood or loss of interest or pleasure. To be defined as a major depressive episode, a symptom must be newly presented or have significantly worsened in comparison to the individual’s pre-episode status. The episode must demonstrate impairment in essential areas of functioning such as social or occupational, or the individual must show significant distress as a result of the episode.
Conversely, if an individual also has a general medical condition such as cancer, diabetes, heart condition or pregnancy, then it can become more difficult to evaluate the symptoms of a major depressive episode as the symptoms can be interchangeable with the symptoms of the medical condition. For example, experiencing fatigue when you are dealing with cancer. Having these symptoms will count towards a major depressive episode unless it can clearly be attributed to the medical condition.
Major Depressive Disorder can occur at any age, but is more prevalent amongst young adults in their 20’s. There are individuals who cannot experience even a month without depression whereas there are others who can be in remission for years but then display the symptoms again later. For 2 in 5 individuals suffering from Major Depressive Disorder, recovery can commence within three months. For 4 in 5 individuals, recovery can begin within 1 year. However, how recent the onset of the individuals’ symptoms is a big factor in determining the likelihood of near-term recovery. Individuals who have been experiencing the symptoms for a shorter length of time are more likely to recover at a faster rate. Other aspects that affect the recovery length include anxiety, personality disorders and how severe the symptoms are.
The longer the time an individual spends in remission, the less likely there is a risk of recurrence. However, the risk of recurrence becomes higher in individuals who are younger, whose prior episodes were severe and whom have previously had persistent depressive episodes.
Risk Factors
- Personal or Family history of Depression
- Early childhood trauma or abuse
- Loneliness and isolation
- Recent stressful life experiences
- Genetic and Physiological
- Alcohol or drug abuse
- Chronic illness or pain
- Financial Hardships
Warning signs
- Decreased work ethic
- Isolating, not contacting people back and staying alone in your room
- Comments about feeling empty, numb or that life will never improve
- Chronic fatigue
- Slowing down in movement or talking
- Restlessness
- Major events, changes or stressors in person’s life
- History of anxiety. Untreated anxiety can lead to depression
- Substance use disorders. People who abuse substances are sometimes doing so to self-medicate the underlying issue of depression.
There are some more warning signs that are more extreme than the ones listed and may need urgent attention. There are many warning signs for suicide, some of which are talking about killing and self-harming, an unusual preoccupation with death, acting recklessly and more. If you notice these warning signs, you may need emergency help.
Comorbidity
There are several other disorders that frequently coincide with Major depressive disorder such as borderline personality disorder, anorexia nervosa, bulimia nervosa, obsessive compulsive disorder, panic disorder and substance related disorders.

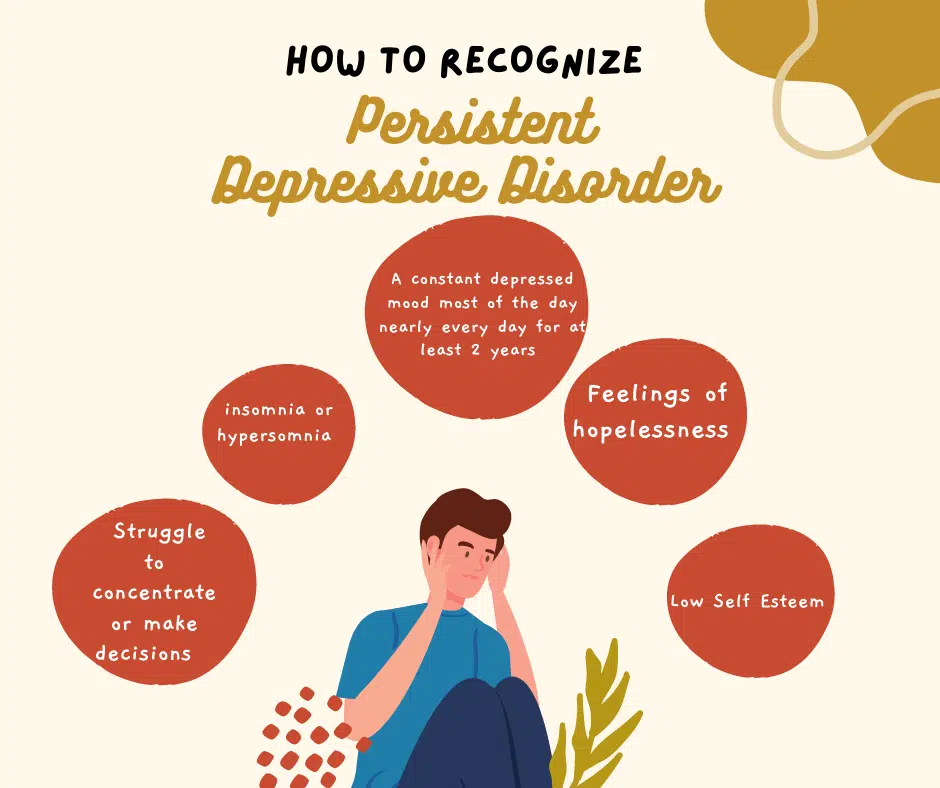
Persistent Depressive Disorder (Dysthymia)
Persistent depressive disorder, also known as Dysthymia, is a chronic form of depression. It can be described as feeling depressed most of the day, almost every day for at least two years. For children and adolescents, these symptoms must be felt for at least one year. It usually has an early onset (childhood, adolescence and young adulthood) and early onset (before 21) is correlated with a higher likelihood of substance disorders and comorbid personality disorders.
The Criteria to Diagnose Persistent Depressive Disorder include:
- A constant depressed mood throughout most of the day, on most days, for at least two years. For Adolescents and children, at least one year.
- Two or more of these symptoms listed below should be present whilst depressed
- Insomnia or Hypersomnia
- Low Self-esteem
- Low Energy or fatigue
- Loss of appetite or overeating
- Feelings of hopelessness
- Struggle to concentrate or make decisions
- During the 2- or 1-year period (for children or adolescents) of depression, the individual has not been without symptom A and B for longer than two months at a time.
- Major Depressive Disorder symptoms may be present continuously for two years.
- A manic or hypomanic episode has never occurred
- The symptoms cannot be attributed to a persistent schizoaffective disorder such as delusional disorder, schizophrenia or another psychotic disorder
- The symptoms cannot be attributed as a side effect to a certain drug or medication or other medical condition such as hypothyroidism.
- The symptoms cause impairment in essential areas of functioning such as social or occupational, or the individual must show significant distress as a result of the symptoms.
Risk Factors
- Having close related family members with major depressive disorder or other depressive disorders
- Negative personality traits such as self-critical, pessimistic and low self esteem
- Traumatic or stress inducing life events
- History of other mental disorders
- Childhood abuse or trauma
Possible Consequences of Persistent Depressive Disorder
- Family conflicts and relationship difficulties
- Decreased productivity in school and work environments
- Reduced quality of life
- Substance abuse
- Suicidal thoughts or recklessness
- Chronic pain
- Anxiety disorders, Major depression and other potential mood disorders
- Other mental health disorders such as personality disorders
Comorbidity
Individuals with persistent depressive disorder are more likely to develop psychiatric comorbidity, particularly anxiety disorders and substance use disorders, than those who have major depressive disorder.
Premenstrual Dysphoric Disorder
Premenstrual Dysphoric disorder causes severe mood shifts which disrupts social or occupational functioning and can damage relationships. The symptoms of irritability and anxiety continuously occur during the pre-menstrual phase of the cycle and diminish around the onset of menses or shortly after. The mood shifts must’ve transpired during majority of the menstrual cycles within the past year and had a significant effect on social or occupational functioning. Other factors which can have an impact on the severity of the symptoms may be due to the cultural and social background of the affected female and other issues such as family perceptions, religious beliefs and social tolerance.
Criteria to diagnose Premenstrual Dysphoric Disorder include:
- During majority of the menstrual cycles, at least five symptoms must be present in the last week before the start of menses, start to get better within the first few days of menses and become insignificant or completely gone the week post menses.
- One or more of the following symptoms must occur:
- Significant irritability, increased anger and/or interpersonal conflicts
- Significant anxiety or tension
- Mood swings
- Self-deprecating thoughts, depressed mood or hopelessness
- To reach a total of five symptoms combined with criteria B, one or more of the following symptoms must also be present:
- Feeling overwhelmed or out of control
- Insomnia or hypersomnia
- Fatigue, lack of energy
- Difficulty in concentrating
- Low interest in activities individual previously used to enjoy
- Change in appetite, overeating, cravings
- Joint or muscle pain, breast tenderness or swelling, feeling bloated or weight gain
- The symptoms cause impairment in essential areas of functioning such as social or occupational, or the individual must show significant distress as a result of the symptoms.
- The symptoms are not due to another disorder such as major depressive disorder, personality disorder
- Criteria A should be confirmed daily with regular observance during at least two cycles
- The symptoms cannot be attributed as side effects to a medication or another medical condition.
Risk Factors
- Genetic and physiological – it is unknown whether premenstrual dysphoric disorder can be hereditary, however premenstrual symptoms are estimated to be 50% heritable.
- Environmental – history of trauma, sociocultural environment, stress and seasonal changes
- Women who take oral contraceptives may experience fewer premenstrual complaints than those who do not.
Comorbidity
The most common reported previous disorder in women who present with premenstrual dysphoric disorder is major depressive disorder. Premenstrual dysphoric disorder should not be diagnosed in situations where an individual only experiences a premenstrual exacerbation of a different mental or physical disorder.

Substance/Medication Induced Depressive Disorder
Substance/medication induced depressive disorder can be characterized as having the same symptoms as major depressive disorder, however the difference is that the depressive symptoms are manifested due to the ingestion of a drug of abuse, medication or toxin. Furthermore, the depressive symptoms continue beyond the anticipated length of physiological effects, withdrawal period or intoxication. The symptoms should start to display within 1 month after use of the substance and/or medication that have the power to trigger the depressive symptoms. Nevertheless, if the depressive disorder symptoms took place before the ingestion or withdrawal from a symptom and/or the depressive disorder symptoms continue to persist beyond a significant amount of time after the termination of substance use, then the diagnosis of substance/medication induced depressive disorder should not be made.
Criteria to diagnose Substance/medication induced depressive disorder:
- A persistent depressed mood and loss of interest in activities
- There is evidence to suggest that criteria A developed during or soon after exposure to medication or substance intoxication or withdrawal. Additionally, the substance/medication in question has the capability to yield those depressive symptoms in criteria A.
- The symptoms cannot be explained by a depressive order that is not induced by medication or substance use
- The symptoms do not manifest solely during a course of hysteria
- The symptoms cause impairment in essential areas of functioning such as social or occupational, or the individual must show significant distress as a result of the symptoms.
Risk Factors
- History of drug/alcohol use
- History of depression
- Types of medication and dosage levels
- More likely to occur within black males with poor educational background and low family income/no insurance.
Comorbidity
Individuals with Substance/medication induced depressive disorder are more likely to have higher rates of comorbidity with any of the DSM 5 mental disorders in comparison to an individual with major depressive disorder and no comorbid substance use disorder. They are also more likely to have antisocial personality disorders, alcohol use disorders and gambling problems. However, individuals with substance/medication induced depressive disorder are less likely to have persistent depressive disorder in comparison to those with major depressive disorder and a comorbid substance use disorder.

Depressive disorder due to another medical condition
What defines depressive disorder due to another medical condition is having the persistent feeling of depressed mood and lack of interest in most activities, but it is regarded as being a direct physiological effect of another medical condition.
A clinician must perform a thorough and comprehensive assessment to produce the conclusion that the depressive symptoms are due to a general medication condition and that the individual indeed has that general medical condition.
Criteria to diagnose Depressive disorder to another medical condition
- A persistent depressed mood and loss of interest in activities
- Evidence through physical examination, laboratory findings and history allude to the fact that the symptoms are a direct consequence of another medical condition.
- The symptoms cannot be alternatively explained by another mental disorder
- The symptoms do not manifest solely during a course of hysteria
- The symptoms cause impairment in essential areas of functioning such as social or occupational, or the individual must show significant distress as a result of the symptoms.
Risk Factors
There are certain medical conditions with which depression is associated such as Parkinson’s disease, Huntington’s disease, traumatic brain injury and stroke. Other conditions that are also closely associated with depression are hypothyroidism and Cushing’s disease.
Comorbidity
Anxiety symptoms are common in depressive disorders and delirium can strike before or along with depressive symptoms in individuals who suffer with a range of medical conditions, such as Cushing’s disease.
Other specified depressive disorder
Other specified depressive disorder applies to when an individual’s symptoms cause impairment in essential areas of functioning such as social or occupational, or the individual shows significant distress as a result of the symptoms. However, the symptoms do not meet the full criteria for the disorders in the depressive disorders diagnostic class. ‘Other specified depressive disorder’ is used when the clinician decides to explain the reason that the symptoms do not meet the criteria for any specific depressive disorder.
Examples of presentations that can be explained using the ‘other specified’ description include:
- Recurrent brief depression: Simultaneous occurrence of depressed mood and at least four other symptoms of depression for a duration of 2-13 days at least once a month for the period of at least one year. The individuals’ symptoms must have never met any criteria for depressive/psychotic/bipolar disorder.
- Short duration depressive episode (4-13 days): Depressed mood and impairment in essential areas of functioning such as social or occupational and at least four out of the other eight symptoms for major depressive episode. These symptoms must persist for more than four days but less than fourteen days. The individuals’ symptoms must have never met any criteria for depressive/psychotic/bipolar disorder and do not meet requirements for recurrent brief depression.
- Depressive episode with insufficient symptoms: Depressed mood and impairment in essential areas of functioning such as social or occupational along with at least one out of the eight symptoms for a major depressive episode. The symptoms must persist for at least two weeks in an individual who has never met any criteria for depressive/psychotic/bipolar disorder and anxiety and depressive disorder symptoms.
Unspecified Depressive Disorder
Unspecified depressive disorder relates to when an individual is experiencing symptoms characteristic of a depressive disorder which is causing impairment in essential areas of functioning such as social or occupational and the individual is demonstrating significant distress due to the symptoms. However, the symptoms do not meet the full criteria for the disorders in the depressive disorders diagnostic class. Therefore, in this situation the clinician is deciding to not specify why the symptoms do not meet the full criteria and instead involves presentations in which there is inadequate information to make a more precise diagnosis.
Specifiers for Depressive Disorder
Specify if:
Individual is presenting with anxious distress. Anxious distress can be described as an individual presenting with at least two of the symptoms listed below during majority of the days they are experiencing persistent depressive disorder or a major depressive episode.
- Restlessness
- Difficulty concentrating
- Tension
- Fear that something untoward may happen
- Fear of losing control of oneself
Specify the severity:
Mild: Two symptoms
Moderate: Three symptoms
Moderate to severe: Four symptoms
Severe: Four or five symptoms
With varied features:
- During majority of the days of a major depressive episode, at least three of the listed hypomanic/manic symptoms are present:
- Reduced need for sleep
- Increased involvement in reckless activities that are more likely to have a negative outcome (e.g., irrational business investments)
- Increase in self-esteem
- Need to be more talkative
- Racing thoughts
- More energetic and goal oriented
- Elevated mood
- These symptoms demonstrate a change in the person’s regular behavior, and it is noticeable to other people.
- The mixed symptoms cannot be because of substance or medication use.
With melancholic features:
- Three of more of the listed symptoms are present during a severe period of a current depressive episode:
- Extreme guilt
- Significant weight loss
- Depression that usually peaks in the morning
- Empty mood
- Waking up at least 2 hours before usual wakening time
- Slowed speech, decreased movement and impaired cognitive function
- One of the following symptoms listed in also present during a severe period of a current depressive episode:
- Loss of interest in almost all activities
- Does not react to when something good happens
Melancholic features are serious, it is not minor depression but is like having a complete absence of happiness or pleasure. There are not many or if any situations that can help improve the individual’s mood.
With atypical features:
This applies when the following symptoms during most of the days of the current or most recent major depressive disorder or persistent depressive disorder.
- Mood improves in reaction to a positive event
- Two or more of the following
- Hypersomnia
- Substantial weight gain or increase in appetite
- Heavy feeling in arms or legs
- Interpersonal rejection sensitivity which impairs ability to function in social settings
Including psychotic features: Delusions/Hallucinations are occurring
With mood-congruent psychotic features: depressive themes such as guilt, disease, deserved punishment and self-inadequacy is the content of the delusions and hallucinations
With mood-incongruent psychotic features: The content of hallucinations/delusions do not contain depressive themes or are a mixture of mood-congruent and mood-incongruent themes.
Other specifiers:
– With catatonia
– With peripartum onset
– With seasonal pattern
Specify if:
In partial remission: Symptoms of previous major depressive episode are present, but the full criteria have not been met or after the episode, there is a period less than two months in which there is no significant symptoms of a depressive episode.
In full remission: no significant symptoms of the disturbance have occurred within the past two months.
Specify current severity:
The severity of the episode depends on the seriousness of the symptoms, the number of symptoms and the effect on functional ability
Mild: Individual possesses few symptoms in excess of those required to determine a diagnosis, the symptoms only have a minor effect on individuals social or occupational functioning and the symptoms are stressful but controllable.
Moderate: The intensity of symptoms, the number of symptoms and the functional impairment is between mild and severe.
Severe: The number of symptoms the individual possesses is significantly higher than those needed to make a diagnosis and the symptoms massively impair social/occupational functioning and are unmanageable and very distressing.

Depression warning signs
There are various warning signs that indicate that maybe you or someone you know may be going through depression. It can be easy to dismiss these signs and/or not take them seriously, but it’s very important to address them when you notice them.
- Decreased work ethic
Noticing that you or someone you know is continuously not putting as much effort as they previously used to into school or work, and that they no longer have the motivation to put hard work into anything.
- Isolating
Preferring to stay alone in your room, preferring to not contact people back when previously the individual was more social.
- Comments about feeling life will not improve
Regular comments along the lines of feeling numb, empty and that life will never get better are something to take notice of.
- Chronic fatigue
Regularly feeling chronic fatigue, tiredness, and sluggishness.
- A slowing down in movement or talking
- Restlessness
Frequent occurrences of anxiety which prohibits the ability to feel properly relaxed or calm
- Major events, changes, or stressors in a person’s life
Take notice when an event such as a family member/close friend passes away or losing a job occurs. These are huge and possibly traumatic events in a person’s life which can be detrimental to their mental health. It is important to observe behavior after these events to try and get help as early as possible if you or someone else is displaying the symptoms of depression.
- History of Anxiety
If you have previously had symptoms of anxiety and have never undergone treatment for it, then this may also be a trigger for depression.
- Substance use disorders
People who abuse substances are at times doing so to self-medicate the underlying issue of depression. It is important to ask and seek help if you or someone you know is abusing substances.
- Increased irritability and agitation
A warning sign most commonly observed in teenage depression.

Depression causes and risk factors
- Genetics and physiology
If your parents dealt with depression, then 2-4x more likely to develop major depressive disorder as its 40% hereditary.
If you suffer from a chronic medical condition such as diabetes, cardiovascular disease, obesity, then you are also more vulnerable to developing depression.
- Environment
Being in chronic stress situations, having social conflicts, having very little social interaction are all common triggers for developing a major depressive episode.

Self-love tips for dealing with depression
- Kind self-talk
Our minds are problem-solving machines and so when we feel depressed, our mind sees it as a problem that it needs to fix. The issue is, sometimes our mind isn’t so kind when going about solving the problem. It is common to find ourselves using harsh words and negative thoughts to try and rid ourselves of depression, but you don’t just tell somebody who is physically sick to just ‘get over it’. In the same sense, you can’t just ‘get over’ or ‘snap out of’ depression.
Kind self-talk is changing the tone we speak to ourselves to be more compassionate and considerate. Consider how you would console a friend who is going through depression and apply it to yourself. Kind self-talk acknowledges the symptoms that we’re experiencing and validates why we act in certain ways due to the symptoms we’re experiencing. It also gives us the opportunity to evaluate our actions and judge whether they are pulling us deeper into depression or helping us to overcome depression. Kind self-talk offers alternative suggestions from a place of love rather than a place of lectures. The alternative suggestion is usually something that the depressive symptoms do not want us to do but advised in a loving and nurturing way. You can also start journaling to reflect on the day and the actions you took in the face of depression from a place of kind self-talk.
- Compassionate imagery
Inner child work
Inner child work is when we imagine ourselves as a very young, innocent child who is suffering and then imagine the ideal version of ourselves today going up to that child to love and support the child. This method is a way of teaching us how to be empathetic to ourselves. The way we treat ourselves and others is usually a learned behavior and so inner child work is a way to reteach ourselves how to give love in the face of pain.
Emotion-based body work
Emotion-based body work is understanding emotional pain and how it lives in our bodies. This includes locating where the emotional pain is in your body, what the texture, color, state is and more. This helps to stay present in your body instead of being pulled by intrusive thoughts and having that snowball effect of emotion. However, we can use imagery to imagine that emotional pain leaving our bodies through a part of our body such as feet, rain washing our pain away or the color of the pain softening. Additionally, it also helps build patience for ourselves and the emotions we are dealing with.
- Kind touch and breathing
Touch is an extremely useful way to calm ourselves down. There are a lot of physiological changes that happen with touch such as activating the parasympathetic nervous system and deactivating the cardiovascular system. This, in turn releases oxytocin in the brain. This is why when you are feeling down and someone gives you a really big hug, you feel a sense of relief.
You can do this for yourself and give yourself a hug, put your hand to your heart, close your eyes and take deep breaths in and out. Additionally, you can give yourself a massage or use a weighted blanket.
- Loving Action
Loving action is going back to the idea of doing the opposite of what the depressive symptoms are pulling us to do. For example, proper exercise, proper rest, eating healthy, surrounding ourselves with company instead of isolating, surrounding ourselves with professionals like therapists, medical doctors who can help you recover from depression.

How to overcome depression
The best way to overcome depression is to put together a super team to help you fight depression. This includes a mental health therapist, psychiatrist, general doctor, and friends & family.
Therapist
A therapist can help you manage your thoughts and emotions that contribute to and prolong depressive symptoms. During counseling, a therapist will help you work through the challenges that are negatively impacting your life and help you formulate strategies and skills to cope with depression and overcome it. The therapist will help you do this by listening, gathering information about you and your history, providing feedback, and working with you to develop the strategies. The main goal of a therapist is to provide you a safe and creative environment to take an emotional risk. Your progress will be tracked, to see when you feel comfortable enough to leave therapy so that you can create a plan for continued progress outside of therapy. [3]
Psychiatrist
Psychiatrists are medical doctors who have extra training in mental health and have many years of study and medical training. You can talk to a psychiatrist about the potential use of medication to manage depressive symptoms at the beginning. A psychiatrist has the medical knowledge to diagnose your condition which in turn enables you to get the right treatment. Additionally, a psychiatrist will figure out which type of psychological treatment and/or medication will work best for you and will know what dosage and strength of medication you may need. If you have alcohol and/or drug problems and/or other conditions such as anxiety, a psychiatrist can help you overcome these through ongoing care and treatment.[4]
General doctor
A general doctor can check for unknown medical conditions that could be causing the depressive symptoms, such as vitamin deficiencies, hypothyroidism, kidney, or liver problems. A GP can also make a general diagnosis and do regular checkups with you to see if your medication is working for you. If your depression is mild, a GP may be the only health professional you need. However, if your depression becomes more severe a GP can refer you to a psychiatrist. If you do use more than one health professional, then it is important for them to communicate with one another on your progress.

Family & Friends
Loneliness and isolation are a symptom and cause of depression. It is important to surround yourself with people you love and trust who will be by your side when you are experiencing depressive symptoms. When you feel alone, it can help to reach out to family and friends who can listen and bring you a sense of company and joy when you’re in a place of darkness.
Wellness recovery action plan
Another way to fight depression is to create an action plan that targets those specific symptoms of a depressive episode that you are experiencing. The wellness recovery action plan helps you to gain insight into your patterns of behavior and develop coping skills so that you can manage your distressing symptoms and have more control over your life. Through the action plan, you can discover more about yourself and learn what helps you and what doesn’t. The plan may also include a crisis plan, in which when you are really struggling and cannot take care of yourself, there is guidance for others on how to take care of you and make the best decisions for you.
Practice Mindfulness
Mindfulness practices are a good way of learning some new skills for dealing with a depressed mood. This is because, through mindfulness practice, we improve our ability to stay present, engage in what we’re doing without judgments, become aware of our thoughts and feelings, and see the depressed mood like a weather pattern passing by. Through mindfulness, you can start to notice the difference between your mood and who you really are.
Doing things that you previously used to enjoy
Another symptom of depression is loss of interest in activities you formerly enjoyed. Humans by nature are social creatures, so you can do the opposite by writing down all the activities you used to enjoy, the people you enjoyed hanging out with, and trying to engage in those things, even if you don’t feel like it.
Good Nutrition
A change in appetite, sometimes with weight loss or weight gain is another common symptom of depression. Getting good nutrition is extremely important as it has an immense impact on your physiology, and it will help you attain the energy you need to deal and manage your depression. Good nutrition consists of a healthy, balanced diet with all the nutrients you need for good physical health.
Activities to promote good sleep
Sleep inconsistencies are also related to depression as many people who suffer from depression note either sleeping too much or too little. To tackle this, you can partake in activities that promote good sleep. These habits can include taking a bath an hour before bedtime, turning off the tv, lighting some candles and putting on calm, relaxing music. All these habits promote good sleep, relaxation and a sense of calmness and will help relax your nervous system to help you get the sleep you need to recover.
Exercise
Feeling slowed down and not having any energy is also common in a depressive episode. Exercise is the best way to combat this symptom. Depression is experienced as an emotion; emotion is literally energy in motion. When you take that energy in motion and you clamp it down within you and don’t let it be in motion, you create this pressure cooker inside and you start to feel it bubbling underneath. As a result, the depressive symptoms are exacerbated when we don’t let that depressed emotion (energy in motion) get released through daily exercise. You can start small with things such as taking a walk and getting fresh air on a regular basis.

Types of therapy for depression
Cognitive Behavioral Therapy (CBT)
CBT is a type of psychotherapy in which you work with a mental health counselor during a limited number of sessions. During CBT, you will identify any traumatic or stressing life events or conditions in your life such as divorce, grief, or a medical condition. You and your therapist will decide which ones you want to work on. When you have recognized the issues, you would like to work on, the therapist will help you become aware of your emotions and thoughts and what you tell yourself and believe about the issue at hand. The therapist will assist you in identifying unhealthy and negative thinking that contributes to your issue and then help you overcome the negative thinking by making you question yourself whether your view of the situation is based on fact or on an inaccurate personal opinion.[5]
Acceptance and commitment therapy and training (ACT)
ACT is a type of cognitive-behavioral therapy and is supported by decades of research. It bases its approach on you understanding what you can and cannot control and taking action based on what works to live a better life. ACT uses mindfulness practices to help handle stress, build confidence, increase performance and deal with all kinds of relationship issues. You will learn three skills to help you notice how you’re feeling about situations:
- Defusion: The ability to disengage from unhelpful thoughts, emotions, beliefs, and memories that are unhelpful to the situation
- Willingness: Making the choice to not fight the difficult thoughts, emotions, urges, experience you are in, so you can handle the situation to the best of your ability
- Presence: Developing the skill to bring yourself back to the here and now every time you get caught up in your head. Using curiosity, openness, and a non-judgmental attitude to ground yourself.

Facts and Resources
Over 300 million people worldwide suffer from depression, so it’s important to understand that you are not alone and there are many routes for help out there. However, if you feel like your depression is too much to handle and you no longer want to live anymore then there are helplines for you to immediately call:
National Suicide Prevention Helpline – 1800-273-8255
SAMHSA Helpline – 1800-662-4357

[1] https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
[2] The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM–5; American Psychiatric Association, 2013)
[3] https://www.mayoclinic.org/tests-procedures/psychotherapy/about/pac-20384616
[4] https://www.mayoclinic.org/diseases-conditions/mental-illness/in-depth/mental-health-providers/art-20045530
[5] https://www.mayoclinic.org/tests-procedures/cognitive-behavioral-therapy/about/pac-20384610
Leave a Reply